SUMMARY: The Medical Biller will be responsible for the day-to-day billing operations of the high volume non-invasive cardiac imaging program within the Division of Cardiology. RESPONSIBILITIES: 1. Verify patient information in IDX Web, Crown, iNYP and Eagle. Work with the Experian Eligibility tool to track insurance verification and referral requirements. Update Experian Eligibility software daily. 2. Update patient account information for resolution on rejected claims on the IDX and/or Crown systems. This includes retrieving patient information from NYP systems, entering patient demographic information, verifying and entering insurance information via the Experian Eligibility system and direct insurance company contacts. 3. Work closely with Phoenix Medcom to perform pre-certifications for procedures and other services, and obtain records and referral information for patient appointments. Obtain referral and/or authorization from the, patient, referring physician, PCP, or the insurance company where applicable. 4. Work claims on the ETM IDX system to address rejections or appeals. 5. Work on all AR rejections that entail invalid patient data, incorrect procedure information, supporting diagnoses, invalid carrier, policy terminations, missing referral/authorizations, credentialing and supporting medical documentation requests. 6. Utilize telephone techniques, patient contact and written correspondence to follow-up with Medicare, Medicaid, Third Party Carriers and patients on outstanding accounts as needed to maximize payments and identify issues. Follow up may be from reports, denials or paperless collection system (IDX). 7. Troubleshoot and identify reimbursement and coding problems. 8. Meet and greet patients and visitors. Serve as a liaison to the clinical staff, answering phones for diagnostic procedures billing questions, perform pre-registration intake for new patients by obtaining the minimum data set, prepare appropriate paperwork for incoming patients. 9. Review all non-invasive cardiac billing encounter forms prior to submission for proper coding, cpt codes, diagnoses, signatures etc. 10. Collect patient payments, insurance payments and co-payments. Maintain a daily log of all cash, check and credit card payments. Work closely with the Billing Coordinator to assist with reconciliation. 11. Submit and reconcile all charges against the schedule. Run weekly missing charge reports. 12. Maintain an inventory of required office supplies and inform the Office Manager of any items needed to order. 13. Ensure patient centered care by demonstrating behaviors that reflect a Culture of Service and will strive to meet the expectations of the “Seven Competencies”. The seven competencies for a “Wow” experience are as follows: 1. Effective Communication 2. Job Knowledge 3. Patient Centered Care 4. Empathy 5. Collaboration and Teamwork 6. Pride and Excellence 7. Integrity and Credibility 14. Conforms to all applicable HIPAA, Billing compliance and safety guidelines. 15. Other duties as required POSITION QUALIFICATIONS: Minimum Education: Bachelor’s degree or the equivalent in education, training and experience in a clinical practice setting Minimum Experience: Knowledge of IDX scheduling systems preferred. Knowledge of Medical terminology and 5 years of related experience Physical Requirements: Must have excellent customer service skills in a high-pressure environment. Must be able to interact with all levels of staff and must have an understanding of patient confidentiality….. Salary $20.00/HR
- Job Seekers
- Employers
- Accounting
- Architecture, Engineering & Construction
- Crypto
- Cybersecurity
- Digital
- Financial Services
- Grant & Fundraising Recruitment
- Healthcare
- Hospitality
- Human Resources
- Legal
- Manufacturing & Engineering
- Mortgage Lending
- Admin Support
- Professional Consulting Services
- Real Estate
- Security Services
- Sports
- Technology
- Diversity Recruiting
- About Us
- Solutions
- Contact Us
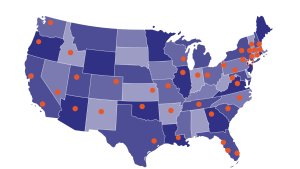
- Locations
- Resource Center

NY Headquarters
1430 Broadway, 13th Floor
New York, New York 10018
877.279.7779
Read our funny (sometimes scary) recruiting tales.